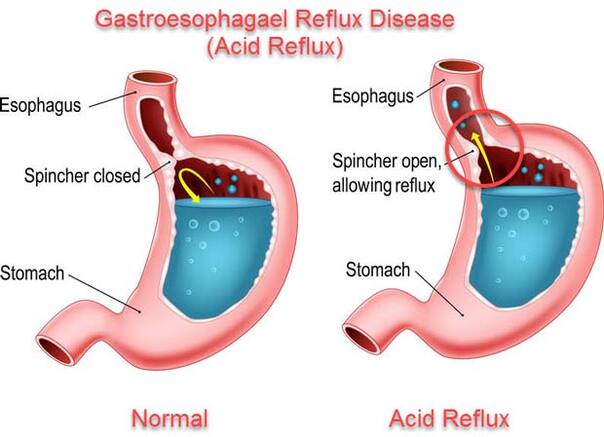
 Heartburn, sometimes referred to as acid reflux, or GERD (gastrointestinal esophageal reflux disease), is one of the most common digestive disorder affecting North Americans. After Lipitor (a cholesterol reducing medication), acid suppressing medications are the most common medication prescribed for this condition. Problems with taking acid suppressing drugs (e.g. nexium, zantac, prilosec):
3 Comments
 Over 50% of women will suffer from a urinary tract infection (UTI) during their lifetime. One-third to one-half of these women will have a recurrent UTI within one year. Recurrent UTI’s are defined as three or more UTI’s in a 12 month period (1). The most commonly used conventional therapies for these conditions are antibiotics. There is increased awareness and concern about antibiotic resistance with repetitive use of these medicines. This growing concern has created an interest in alternative treatments for UTI’s. The purpose of this article is discuss this conditions, the causes, and alternative treatments for cure and further prevention. This article will also illuminate the link between UTI’s and an imbalanced gut microbiome, otherwise known as dysbiosis. Gastrointestinal conditions associated with dysbiosis such as Irritable Bowel Syndrome (IBS) and Small Intestine Bacterial Overgrowth (SIBO) are common in those with bladder infections.  Bloating is not fun. We've all been through it, looking 9 months pregnant can make us feel unpleasant, uncomfortable and unattractive. Bloating can come with other symptoms like constipation, gas, stomach or lower abdominal pain, feeling swollen and more. So what causes bloating? Here are 6 of the most common causes of bloating I see in practice. 1. Eating Habits - eating or drinking too quickly, eating too much food, not properly chewing our food can result in bloating. The reason for this is that our body is not able to secrete the proper amount of enzymes and stomach acid to effectively break down our food. Another reason is that eating too quickly increases the likelihood of swallowing air. Take away: eat mindfully, do not have liquids with your meal, and watch your portions. I really like the 5-10-15 rule: take 5 deep belly breaths before a meal, put down your utensils for 10 seconds after every bite, and make sure your meal takes no less than 15 minutes.  Part 1 - Your Digestion from an Eastern Perspective According to naturopathic medicine, our digestive system is the key to balanced health and vitality. Naturopathic medicine is a combination of Western, modern scientific knowledge with Eastern traditions. Eastern traditions include: Traditional Chinese Medicine (TCM), which was the first formalized system of healthcare in modern civilization, along with Ayurvedic Medicine, the ancient medical system from India. Both of these traditions understand that in order to extract the nourishment we need from food, there needs to be balance and integrity in both the body and mind.  Constipation is a condition that affects 1 in 4 Canadians and is defined as having a bowel movement fewer than four times per week. Chronic constipation can sometimes be managed with diet and lifestyle including extra fluid intake, exercise, increased dietary fibre and more. For some of us though, these changes either make a small difference or the effect doesn’t last and the constipation returns! |
AuthorDr. Lara is a Naturopathic Doctor who is passionate about helping and empowering her patients in their journey towards lifelong health and wellness Categories
All
Archives
September 2021
|